In this web journal post, we’ll dig into 10 Common skin infections requiring prompt consideration. And also we’ll outline symptoms and treatment options for each, empowering you to initiate your healing journey.
Common skin infections:
1 Eczema (Atopic Dermatitis)
2. Acne (Acne Vulgaris)
3. Shingles (Herpes Zoster)
4. Hives (Urticaria)
5. Sunburn
6. Contact Dermatitis
7. Diaper Rash
8. Rosacea
9. Athlete’s Foot (Tinea Pedis)
10. Basal Cell Carcinoma

Eczema (Atopic Dermatitis)
If your skin feels dry, itchy, and red, you might have eczema, also known as atopic dermatitis. It’s a Common skin infections that isn’t contagious. Individuals who have asthma or sensitivities are more likely to urge it there isn’t a remedy. While there are medications to assist with the side effects, there isn’t a remedy.
Why Does Eczema Happen?:
Eczema, Acne, Shingles, etz are the Common skin infections.
Dermatitis, also known as atopic dermatitis, may be a skin condition characterized by dry, bothersome, and aroused skin.
While the exact cause of eczema remains unclear, researchers believe that a combination of genetic, environmental, and immune factors contribute to its development.
Let’s explore the key factors that may trigger eczema.
Genetic Predisposition:
Genes are important in eczema. If someone in your family has eczema, asthma, or allergies, you might get it too. Some specific gene differences related to how your skin works and how your immune system reacts can make you more likely to have eczema.
Immune System:
In eczema, the immune system doesn’t work properly. It gets too sensitive to things like allergens or irritants. This makes the skin get red, swollen, and itchy. Fixing how the immune system works could lead to new treatments for eczema.
Skin Barrier Dysfunction:
In eczema, the skin’s protection isn’t as good as it should be. This lets things like allergens, germs, and other things bother the skin more easily, causing redness and swelling. Fixing the skin’s protection is really important to make eczema symptoms better and stop them from coming back.
Environmental Triggers:
Things in the environment like allergens, irritants, and dirt can make eczema worse. Common things that can make it worse are dust mites, pet hair, pollen, strong soaps, and certain kinds of clothes. It’s important to figure out what makes eczema worse and try to avoid those things to help manage it and make the symptoms less severe.
Symptoms of Dermatological conditions
Here are many common signs to take care for: Here are a couple of signs to watch out for:
Itchy Skin:
One of the hallmark symptoms of eczema is intense itching, which can be relentless and disruptive, especially at night.
Dry, Red, or Inflamed Skin:
Eczema often causes patches of dry, red, or inflamed skin that may appear rough or scaly. These patches can occur anywhere on the body but are commonly found on the hands, arms, elbows, knees, and face.
Rash:
Eczema may manifest as a rash consisting of small, raised bumps that may ooze fluid and crust over when scratched. The rash can be widespread or localized to specific areas of the body.
Skin Discoloration:
In some cases, eczema patches may lead to changes in skin color, ranging from lighter to darker shades than the surrounding skin.
Thickened Skin:
Prolonged scratching and rubbing of eczema-affected skin can lead to thickened areas known as lichenification. These patches may feel rough and leathery to the touch.
Sensitivity to Irritants:
People with eczema often have heightened sensitivity to irritants such as soaps, detergents, fragrances, and certain fabrics, which can trigger or exacerbate symptoms.
Cracked or Broken Skin:
Severe eczema may cause the skin to become cracked, broken, or prone to infection, leading to pain and discomfort.
Effective Solutions for Skin disorders:
“Common skin infection”If you’re dealing with eczema, it’s best to reach out to a doctor for help rather than trying to manage it alone. Here’s why:
Accurate Diagnosis:
Doctors can identify eczema and make sure it’s not another skin problem This helps you get the correct treatment.
Personalized Care:
They’ll create a treatment plan just for you based on your symptoms, triggers, and medical history.
Tackling Triggers:
Even if you can’t change things like genetics, doctors can help you find and manage triggers that make eczema worse, like certain products or stress.
Conclusion:
Understanding the triggers and symptoms of eczema” Common skin infections” is key for effective management. Seeking professional medical advice ensures accurate diagnosis and personalized treatment plans. With proper care, individuals can alleviate discomfort and prevent exacerbations of this common skin condition.
more about Atopic Dermatitis

Acne:Epidermal infections
Acne, also called acne vulgaris, is a Common skin infections that happens when pores get congestedwith oil and dead skin cells. This can make pimples, blackheads, and whiteheads appear, along with red, swollen bumps called papules and pustules.
Acne can show up on your face, neck, chest, back, and shoulders, often starting during puberty because of hormone changes. While it’s not usually a serious health issue, acne can be uncomfortable, embarrassing, and upsetting for people who have it. Treatments for acne include creams, pills, and lifestyle changes to reduce oil and inflammation.
Eczema, Acne, Shingles, etz are the Common skin infections.
Why Does Acne Happen?:
Acne is something a lot of people deal with, especially when they’re teenagers. Here’s why it shows up:
Too Much Oil:
Our skin makes oil to keep it hydrated. Sometimes, though, it makes too much, which can block our pores.
Pore Blockage:
: When dead skin mixes with extra oil, it plugs up the pores. This makes a perfect place for bacteria to grow.
Bacteria Growth:
Tiny bacteria called P. acnes live on our skin. When pores are blocked, these bacteria multiply, causing redness and swelling.
Hormonal Changes:
: When hormones go haywire during puberty, periods, pregnancy, or when we’re stressed, they can make our skin oilier and trigger acne.
Family Traits:
: If your family members had acne, you might get it too. Sometimes it’s just in our genes.
Food Choices:
: Some studies suggest that certain foods, like sugary stuff or dairy, might make acne worse for some people. But we’re still learning about this.
Bad Products:
Using makeup or skincare stuff that blocks pores or irritates the skin can make acne worse. It’s better to choose products that won’t clog pores.
Skin Rubbing:
: Things like tight clothes or touching our face a lot can make acne worse by rubbing the skin and spreading bacteria.
So, acne happens because of too much oil, blocked pores, bacteria, hormones, genes, and some lifestyle stuff. To treat it, we need to take care of our skin, make some changes in our lifestyle, and sometimes get help from a doctor.
Symptoms of Cutaneous infections :
Acne is Common skin infections can look different depending on how bad it is:
Whiteheads: These are closed pores filled with gunk.
Blackheads: These are open pores filled with gunk.
Red Bumps: Small bumps that are red and tender.
Pimples: Bumps with pus at the top.
Big, Painful Lumps: Solid, painful bumps under the skin.
Pus-filled Lumps: Painful lumps under the skin filled with pus.
Acne usually shows up on the face, forehead, chest, upper back, and shoulders.is
Effective Solutions for Relief:
Dealing with acne? Here are some things you can try to feel better:
Keep It Clean:
Wash your face twice a day with a gentle cleanser to remove dirt and oil. Don’t drop too hard, though—it can make things worse.
Don't Squeeze:
Use skincare products labeled “non-comedogenic” or “oil-free” to avoid congesting pores. And don’t overstate it—too many products can irritate your skin.
Hands Off:
Try not to touch your face too much. Our hands carry a lot of dirt and bacteria that can make acne worse.
Remain Hydrated:
: Drinking bounty of water can offer assistance flush out poisons and keep your skin hydrated.
Healthy Diet:
While the link between diet and acne isn’t crystal clear, eating a balanced diet with lots of fruits and veggies can’t hurt. Some people find that cutting back on sugary foods helps.
Manage Stress:
: Stress can spark acne flare-ups, so find ways to relax and decompress —whether it’s through exercise, contemplation, or spending time with loved bones.
Visit a Dermatologist:
: If home remedies aren’t cutting it, don’t vacillate to see a dermatologist. They can define specifics or treatments acclimatized to your skin’s requirements.
Keep in mind, everyone’s skin is distinctive, so what works for one existent might not work for another. Be patient and gentle with your skin, and don’t be afraid to seek professional help if you need it.
Conclusion:
Acne is a commons skin infection caused by factors like excess oil, pore blockage, bacteria, hormones, genetics, and lifestyle. Treatments include skincare, lifestyle changes, and professional guidance. Remember, everyone’s skin is unique, so patience and personalized care are key to managing acne effectively.
more about Acne

Shingles (Herpes Zoster)
Shingles is a sickness where you get a rash or blisters that hurt. It’s caused by a virus called varicella-zoster virus (VZV), which is the same virus that gives you chickenpox. The rash usually shows up in a strip or patch on one part of your body.Eczema, Acne, Shingles, etz are the Common skin infections.
Why does Shingles (Herpes Zoster)Happen?:
Shingles comes from the same germ that causes chickenpox. Once you get chickenpox, the germ stays inside you. Later on, it might wake up and cause shingles. Most people only get shingles once. The germ can wake up because you’re older, feeling stressed, sick, or taking certain medicines. Sometimes, we don’t know why it wakes up.
Symptoms of this Skin maladies :
Shingles can start with these early symptoms:
Fever: You might feel hot and have a temperature.
Chills: You may shiver or feel cold.
Headache: Your head might hurt.
Feeling Tired: You might feel more exhausted than usual.
Sensitivity to Light: Your eyes may feel uncomfortable in bright light.
Stomach Upset: Your stomach might feel upset or queasy.
Other Signs and Symptoms:
After these early signs, you might notice:
Itching, Tingling, or Burning: Your skin in a certain area might feel strange.
Redness: The affected area of your skin could turn red.
Raised Rash: You might see a rash that’s bumpy or raised.
Blisters: Small blisters filled with fluid might appear, then burst and scab over.
Pain: The skin in that area might hurt a little or a lot.
Duration of Shingles Outbreak:
Shingles doesn’t vanish overnight. It can stick around for a while, usually lasting from three to five weeks.
1. Early Signs:
Before the rash shows up, you might feel discomfort on your skin. It could be itchy, burning, or even like sharp painsThis more often than not begins a number of before the hasty shows up.
2. The Rash Arrives:
Then, you’ll see a raised rash forming. It might look like a band or a patch, typically on just one side of your body. It commonly shows up around your waist, on your face, neck, or trunk, but it can pop up elsewhere, like on your arms or legs.
3. Blisters and Pain:
Within a few days, the rash turns into red blisters filled with fluid. These can be pretty painful and uncomfortable.
4. Drying Out:
After a while, usually around 10 days, the blisters start to dry up and form scabs.
5. Healing Time:
It takes a bit longer for those scabs to disappear—around two to three weeks.
So, from start to finish, dealing with shingles can take some time, but knowing what to expect can help you manage it better.
Effective Solutions for Relief:
Here’s what can help when you have shingles:
Medicine to Fight the Virus:
Your doctor might give you antiviral pills. They fight the virus and make the rash better faster. It’s best to take them as soon as you see the rash.
Relieving Pain:
It’s important to make the pain less. You can take pain pills like acetaminophen or ibuprofen. Sometimes, you might need stronger pills or numbing cream from the doctor.
Eye Drops (if eyes are affected):
If shingles hurt your eyes, the doctor might give you special drops or ointment to keep them safe.
Keeping the Rash Clean:
You need to keep the rash clean and dry. Wash it gently with soap and water. Putting cool cloths on it can make it feel better.
Using Special Lotions or Baths:
To stop the itchiness, you can use special lotions like calamine or have baths with oatmeal.
Rest and Take Care of Yourself:
It’s vital to rest and watch out of yourself.Don’t scratch the rash because it can make it worse and leave scars.
Get Vaccinated:
If you’re 50 or older, getting the shingles vaccine can help prevent future outbreaks or serious problems.
Conclusion:
Shingles, caused by the varicella-zoster virus, results in a painful rash or blisters typically in a strip or patch on the body. While triggers can vary, factors like age and stress can awaken the dormant virus from previous chickenpox infection. Symptoms include fever, headache, fatigue, and skin sensitivity, followed by itching, redness, blisters, and pain. Treatment involves antiviral medication, pain relief, and keeping the rash clean. Vaccination for individuals over 50 can help prevent future outbreaks.
more about Shingles
Hives (Urticaria):
“Hives, also known as Urticaria – hives. It happen to about 20 percent of people sometime in their lives.Hives are raised, often itchy, red bumps (welts) on the surface of the skinThey can be an unfavorably susceptible response to nourishment or pharmaceutical. It is common skin infections.
They can also appear without cause. They can come from different things like allergies to foods, medicines, bug bites, or stuff in the air like pollen or pet fur. When hives start, your skin might feel itchy, then turn into red, raised bumps. These bumps can be small or big and can show up and vanish in a few hours, or stick around for days or weeks. Even though hives usually go away on their own and aren’t harmful, they can make you feel uncomfortable and upset. Eczema, Acne, hives, etz are the Common skin infections.
Why does Hives (Urticaria) Happen?
Hives, also called urticaria, “Common skin infections” occur for various reasons:
**Allergies:** Your body may react to certain foods, medications, insect stings, or environmental factors like pollen or pet dander.
**Infections:** Viral or bacterial infections can trigger hives in some individuals.
**Physical Factors:** Exposure to extreme temperatures, pressure on the skin (such as from tight clothing), or sun exposure can lead to hives.
**Stress:** Emotional stress or anxiety can sometimes cause hives to appear.
**Underlying Health Conditions:** Certain medical conditions like autoimmune disorders or thyroid problems may be associated with chronic hives.
**Genetic Factors:** Hives can sometimes run in families, suggesting a genetic predisposition to the condition.
**Unknown Triggers:** In many cases, the exact cause of hives remains unknown, and they occur without any identifiable trigger.
Understanding these potential triggers can help manage and prevent hives outbreaks in some cases. However, individual responses to triggers vary, and what causes hives in one person may not affect another. If you experience hives frequently or have difficulty identifying triggers, consulting a healthcare professional can provide guidance on managing your condition effectively.
Symptoms of common skin infections:
Itching:
One of the hallmark symptoms of hives is intense itching. This itching sensation can be persistent and aggravating, leading to considerable discomfort for individuals experiencing hives.
Swelling of the Skin:
Hives typically present as raised welts on the surface of the skin. These welts can vary in color, appearing red or skin-colored, and often have clearly defined edges. The swelling can range from mild to severe, depending on the individual’s reaction.
Formation of Wheals:
The raised welts, known as wheals, may enlarge, spread, or merge together, forming larger areas of raised skin. These wheals can be flat or slightly raised and may evolve in shape and size over time.
Rapid Changes in Appearance:
One distinctive characteristic of hives is their transient nature. Wheals can appear suddenly, change shape, disappear, and reappear within minutes or hours. It is uncommon for a wheal to persist for more than 48 hours, making hives an unpredictable and dynamic condition.
Dermatographism:
A unique form of hives known as dermatographism or “skin writing” occurs in response to pressure on the skin. When the skin is pressed or scratched, immediate hives develop in the affected area, creating raised welts resembling the pattern of the pressure applied.
Recognizing these symptoms is crucial for identifying and managing hives effectively. While hives typically resolve on their own and are not usually a cause for concern, persistent or severe symptoms may warrant medical attention. Counseling a health care proficient can offer assistance decide the basic cause of hives and give suitable treatment and alleviation for those influenced
Effective Solutions for Relief:
If you’re dealing with mild hives, you might not need treatment as they can go away by themselves. But if you’re feeling itchy or swollen, here are some things you can do to feel better:
Avoid Hot Baths or Showers:
Hot water can make hives worse, so stick to lukewarm or cool water when bathing.
Wear Loose Clothes:
Tight clothing can rub against your skin and make hives more irritating. Opt for loose-fitting outfits to give your skin some breathing room.
Try Antihistamines:
Your doctor might recommend taking antihistamine medicines like Benadryl or Zyrtec to help with itching and swelling. Just make sure to follow the instructions on how to take them.
Consider Prescription Medications:
In some cases, especially if you have long-lasting hives, your doctor might prescribe other medicines to help manage your symptoms.
Seek Urgent Help if Needed:
If your hives are severe, especially if your throat is swelling up, it’s crucial to get emergency medical attention. In these cases, you might need a shot of epinephrine (adrenaline) or steroids to prevent breathing problems caused by throat swelling.
Taking these simple steps can help ease the discomfort of hives and get you back to feeling like yourself again. Remember to consult with your healthcare provider for personalized advice and treatment options tailored to your needs.
Conclusion:
In summary, hives, or urticaria, are red, itchy bumps on the skin caused by various factors like allergies, infections, or stress. While they typically resolve on their own, they can be uncomfortable. Managing hives involves avoiding triggers, taking antihistamines, and seeking medical attention if severe. all of ten are Common skin infections.
more about Hives

Sunburn:
Sunburn happens when your skin gets too important sun. This can make your skin red, sore, and hot to the touch. It generally shows up within a many hours of being in the sun too long, but occasionally it might take up to a day. sunburn, Acne, Shingles, etz are the Common skin infections.
Why does Sunburn Happen:
Sunburn is caused by spending too important time in the sun’s shafts. These shafts have commodity called ultraviolet( UV) radiation, which can hurt your skin. When your skin gets too important UV radiation, it gets bothered and lit . This is what makes your skin red, painful, and hot.
Symptoms:
When you have sunburn, “these are common skin confitions” you might notice Red Skin On lighter skin, sunburn makes the skin look pink or red.
On darker skin, it might be harder to see, but the skin can still get darker or change color.
Feeling on Your Skin Sunburned skin feels warm or hot because it’s swollen. It can also feel painful, tender, or itchy.
Swelling Sunburn can make the skin swell over, which can feel uncomfortable.
Pocks occasionally, sunburn causes little pocks filled with fluid to appear on the skin.
still, it can make the skin more prone to infection and take longer to heal, If these pocks break.
Other Signs still, you might feel sick each over, If the sunburn is really bad.
This can include having a headache, fever, feeling squeamish, or being veritably tired.
Eye Problems still, your eyes might hurt or feel gritty, If you spend too important time in the sun.
Effective Solutions for Relief:
In this article, we’ll explore some easy methods to soothe sunburned skin using items you may already have at home.
Cool Compresses:
When your skin feels hot from sunburn, cool compresses can help.
Here’s how:
Take a clean cloth and splash it in cold water. Gently place the cold cloth on the sunburned area for 10-15 minutes at a time.
Aloe Vera Gel:Aloe vera is a plant known for its soothing properties and can be helpful for sunburn.
Here’s what you can do:Apply pure aloe vera gel directly onto the sunburned skin.
You’ll keep the aloe vera gel within the fridge for an extra cooling sensation some time recently utilize.
Hydration:
Sunburn can make your skin feel dry, so it’s important to drink plenty of water.
Here’s why: Drinking at slightest 8 glasses of water a day can offer assistance keep your skin hydrated from the interior out.
If your sunburn is severe, consider drinking even more water to help with symptoms.
Moisturizers:
Using moisturizers can help keep your sunburned skin from drying out further.
Here’s what to look for: Choose gentle moisturizers that don’t have added scents or fragrances.
Look for ingredients like ceramides, hyaluronic acid, or shea butter to help repair your skin.
Oatmeal Bath:
Oatmeal can help soothe sunburned skin and relieve itching.
Here’s how to form an oats shower: Add one cup of finely ground oatmeal to a bathtub filled with lukewarm water.
Soak in the oatmeal bath for 15-20 minutes to help calm your skin.
Pain Relievers:
If your sunburn is causing you pain, over-the-counter pain relievers can help.
Here’s what you need to know: Ibuprofen or acetaminophen can help reduce sunburn pain and inflammation.
Follow the dosage instructions on the package, and talk to a doctor if you’re unsure.
Avoid Further Sun Exposure:
To prevent your sunburn from getting worse, it’s important to protect your skin from more sun exposure.
Here’s how: Stay indoors or cover up with clothing and hats when you’re outside.
If you have to be in the sun, use a sunscreen with SPF 30 or higher to protect your skin.
Conclusion:
Sunburn occurs when skin is exposed to excessive UV radiation, leading to redness, soreness, and discomfort. Remedies include cool compresses, aloe vera, hydration, moisturizers, oatmeal baths, and pain relievers. To prevent worsening, avoid further sun exposure and use sunscreen.all of ten are Common skin infections.
more about Sunburn

Contact Dermatitis:
Contact dermatitis is when your skin gets red, itchy, and blown because it touched commodity it did not like. This could be anything from cleaner or soap to shops like bane ivy. occasionally, it happens because you are antipathetic to commodity you touched.
Why Contact Dermatitis Happens:
Contact dermatitis is when commodity touches your skin and makes it reply. This response can beget your skin to come red, itchy, and swollen. It’s like your skin’s way of saying it does not like what it touched.Eczema, Acne, Shingles, etz are the Common skin infections.
Symptoms:
Itching:
Contact dermatitis makes your skin feel veritably itchy, and scratching can make it worse.
Greenishnesss:
Contact dermatitis is when commodity touches your skin and makes it reply. This response can beget your skin to come red, itchy, and swollen. It’s like your skin’s way of saying it does not like what it touched.
Rash:
You might get bumps, pocks, or dry patches on your skin where the rash is.
Swelling:
: occasionally, the area with the rash can swell up and feel puffy.
Pain or Burning:
The rash might make your skin feel sore or like it’s burning.
Effective Solutions for Relief:
To stop the itching and reduce redness, try using a cream or ointment that you can buy at the store. Look for one with 1% hydrocortisone, which can help calm your skin down. You can also try putting it in the fridge before using it for a cooling effect. Another option is calamine lotion, which can also help with itching and soothe your skin.
Take Oral Antihistamines:
If you’re having trouble sleeping because of itching, an antihistamine pill can help. These are medicines that can reduce itching and make you feel more comfortable. Make sure to follow the instructions on the package or ask your doctor for advice.
Apply Cool, Wet Compresses:
To help your skin feel better, try putting a clean, wet cloth on the rash for 15 to 30 minutes a few times a day. This can reduce swelling and itching and make you feel more comfortable.
Protect Your Skin:
Try not to scratch your rash, as this can make it worse and increase the chance of infection. Keep your nails short to avoid scratching, and cover the rash with a bandage if you need to. Also, make sure to protect your skin from the sun by wearing sunscreen or covering up with clothes.
Soothing Cool Baths:
Taking a cool bath with oatmeal can help calm your skin and make you feel better. Try adding an oatmeal-based product to your bathwater and soaking for about 20 minutes.
Hand Care:
If your hands are affected by contact dermatitis, be extra careful to take care of them. Wash and dry your hands well, and use moisturizer throughout the day to keep them hydrated. If you need to protect your hands, wear gloves made of materials like plastic lined with cotton.
Conclusion:
Contact dermatitis causes red, itchy, and swollen skin due to exposure to irritants or allergens. Relief methods include using creams, taking antihistamines, applying cool compresses, protecting the skin, taking oatmeal baths, and practicing hand care. Avoid scratching to prevent worsening symptoms and promote healing.
more about Contact Dermatitis

Diaper Rash:
Diaper rash is a type of dermatitis characterized by red, irritated patches of skin in the diaper area. It typically occurs when a baby’s skin is exposed to wet or soiled diapers for dragged periods, leading to irritation and inflammation. Additionally, friction from chafing and sensitivity to certain diaper materials or products can contribute to the development of diaper rash.
Why Diaper Rash Happens:
Diaper rash can do when the pH of the skin changes, making it more alkaline or basic. Additionally, enzymes from baby’s stool can come more active, leading to tissue and skin damage. Understanding these processes can help parents take proactive steps to help diaper rash. Eczema, diaper rush, Shingles, etz are the Common skin infections.
The Role of Urine:
Diaper rash can do when the pH of the skin changes, making it more alkaline or basic. Additionally, enzymes from baby’s stool can come more active, leading to tissue and skin damage. Understanding these processes can help parents take proactive steps to help diaper rash.
The Role of Urine:
When a baby urinates in their diaper, the urine breaks down and releases ammonia. Ammonia is a compound that can increase the pH of the skin, making it more basic. As the pH of the skin rises, it becomes more susceptible to irritation and damage.
The Effect of Stool Enzymes:
Enzymes present in baby’s stool can also contribute to diaper rash. These enzymes come more active as the pH of the skin rises, leading to increased breakdown of tissues and skin damage. This can further complicate the symptoms of diaper rash and protract healing time.
precluding Diaper Rash:
precluding diaper rash involves maintaining a healthy pH balance of the skin and minimizing exposure to urine and stool enzymes. Here are some tips for precluding diaper rash:
Change diapers frequently to reduce exposure to urine and stool.
Cleanse the diaper area gently with mild soap and water during diaper changes.
Allow the skin to state dry completely before putting on a fresh diaper.
Apply a barrier cream or ointment to cover the skin from moisture and irritation.
Use diapers and wipes free of fragrances and harsh chemicals to minimize skin irritation.
Symptoms:
Ruddy, kindled patches of skin within the diaper range .
Irritability or discomfort during diaper changes
Fussiness or crying, especially during diaper changes
Skin sensitivity or tenderness to touch
Effective Solutions for Relief:
Keep the Diaper Area Clean and Dry:
Change diapers frequently: To prevent prolonged exposure to moisture, aim to change your baby’s diaper every few hours, or as soon as it becomes wet or soiled.
Gently cleanse the diaper area: During diaper changes, use mild soap and water or baby wipes to gently clean your baby’s skin.
Avoid wipes containing alcohol or fragrances, as they can cause irritation.
Pat the skin dry: After cleaning, pat the skin dry with a soft, absorbent cloth or allow it to air dry completely before putting on a fresh diaperMaintain a strategic distance from rubbing or cleaning, as this could encourage aggravate the skin
Use Barrier Creams or Ointments:
Apply a thick layer of barrier cream or ointment: To protect your baby’s skin from moisture and irritation, apply a generous amount of barrier cream or ointment to the diaper area during each diaper change.
Look for products with protective ingredients:
Choose barrier creams containing zinc oxide or petroleum jelly, as they create a protective barrier on the skin to prevent irritation and promote healing.
Give Diaper-Free Time:
Allow your baby to go diaper-free: Giving your baby some diaper-free time each day allows their skin to breathe and helps prevent diaper rash.
Lay your baby on a waterproof pad or towel to catch any accidents.
Monitor your baby: During diaper-free time, keep a close eye on your baby to prevent messes and ensure their safety.
Avoid Potential Irritants:
Choose diapers and wipes wisely: Opt for diapers and wipes that are free of fragrances, dyes, and harsh chemicals, as these can irritate your baby’s delicate skin.
Skip the baby powder: Avoid using baby powder, as it can be inhaled by your baby and further irritate their skin.
Stick to gentle cleansers and barrier creams instead.
Conclusion:
Diaper rash is a common skin condition caused by exposure to wet diapers, friction, and sensitivity to products. Prevention involves frequent diaper changes, gentle cleansing, using barrier creams, giving diaper-free time, and avoiding irritants. By following these tips, parents can effectively manage diaper rash and ensure their baby’s comfort.
more about Diaper Rash
Rosacea:
Rosacea may be a skin condition that fundamentally influences the confront, causing redness, flushing, and obvious blood vessels. It may also lead to the development of small, acne-like bumps or pustules on the skin. Rosacea symptoms often flare up for weeks or months before subsiding temporarily.
Why Rosacea Happens:
Rosacea may be a skin condition that fundamentally influences the confront, causing redness, flushing, and obvious blood vessels. It may also lead to the development of small, acne-like bumps or pustules on the skin. Rosacea symptoms often flare up for weeks or months before subsiding temporarily. (Eczema, rosacea, Shingles, etz are the Common skin infections.)
Symptoms:
Facial Redness and Flushing:
One of the hallmark symptoms of rosacea is facial redness and flushing. People with rosacea may notice that their face flushes more easily, and over time, the redness may become more persistent. Depending on skin color, the redness may appear subtle or more pronounced, ranging from pink to purple in hue.
Visible Veins:
Rosacea can cause small blood vessels on the nose and cheeks to break and become larger, resulting in visible veins. These veins, also known as spider veins, may be subtle and challenging to see, especially in individuals with darker skin tones.
Swollen Bumps:
Many individuals with rosacea develop swollen bumps on the face that resemble acne. These bumps may contain pus and can appear on the nose, cheeks, chin, and forehead. In some cases, they may also occur on the chest and back, contributing to discomfort and self-consciousness.
Burning Sensation:
The affected area of the skin may feel hot, tender, or irritated, resembling a burning sensation. This discomfort can vary in intensity and may worsen during rosacea flare-ups.
Eye Problems:
Ocular rosacea is a common complication of rosacea characterized by dry, irritated, and swollen eyes and eyelids. Some individuals may experience eye symptoms before, after, or concurrently with skin symptoms, highlighting the importance of addressing both aspects of the condition.
Enlarged Nose:
In some cases, rosacea can lead to thickening of the skin on the nose, resulting in a condition known as rhinophyma. Rhinophyma causes the nose to appear enlarged and bulbous, primarily affecting men more than women.
Effective Solutions for Relief:
When to Seek Professional Help:
If your rosacea symptoms persist or worsen despite following self-care tips,
it’s essential to consult a member of your healthcare team.
Signs that you simply require proficient treatment include:Signs merely may require proficient treatment incorporate:
Persistent facial redness, flushing, or swelling
Frequent flare-ups or worsening of symptoms
Development of swollen, pus-filled bumps
Eye irritation or other ocular symptoms associated with rosacea
Thickening of the skin on the nose (rhinophyma)Thickening of the skin on the nose (rhinophyma).
Prescription Medications:
Your healthcare provider may prescribe topical gels or creams containing medications such as metronidazole, azelaic acid, or sulfur to help reduce inflammation and control symptoms. These medications can be applied directly to the affected areas of the skin and may provide relief from redness, swelling, and irritation.
In some cases of more severe or persistent rosacea, oral medications such as antibiotics or isotretinoin may be prescribed. These medications work to reduce inflammation and prevent flare-ups by targeting the underlying causes of rosacea.
Conclusion:
Rosacea manifests as facial redness, visible blood vessels, and acne-like bumps, often causing discomfort and self-consciousness. Effective management involves self-care strategies and professional treatment when necessary, helping individuals alleviate symptoms and improve their quality of life.
more about Rosacea
Athlete’s Foot (Tinea Pedis):
Athlete’s foot is a fungal infection primarily affecting the skin on the feet. It’s caused by various types of fungi, which thrive in warm and moist environments, such as sweaty socks and shoes. The fungus can easily spread from person to person through direct contact or by walking barefoot in contaminated areas like locker rooms and communal showers.
Why Athlete’s Foot Happens:
Firstly, athlete’s foot is caused by fungi. These fungi are everywhere around us, but they particularly love warm and damp places. When our feet get sweaty and are confined in tight shoes, it creates the perfect environment for these fungi to thrive. That’s why it often starts between the toes, where moisture tends to linger.(Eczema, Acne, Shingles, etz are the Common skin infections.)
Symptoms:
Textured, Peeling, or Split Skin Between the.
One of the classic signs of athlete’s foot is the presence of scaly, peeling, or cracked skin between your toes. This happens because the fungus thrives in warm, moist environments, like the spaces between your toes, leading to irritation and skin damage.
Persistent Itchiness, Especially After Removing Shoes and Socks
Do you find yourself scratching your feet incessantly, especially right after taking off your shoes and socks? Itchiness is a hallmark symptom of athlete’s foot. The fungus irritates the skin, triggering an urge to scratch and providing temporary relief that soon leads to more irritation.
Inflamed Skin with Reddish, Purplish, or Grayish Discoloration
Inflamed skin is another common indicator of athlete’s foot. Depending on your skin color, the affected areas may appear reddish, purplish, or grayish. This discoloration is a result of the body’s immune response to the fungal infection and can vary in intensity.
Burning or Stinging Sensation
If you experience a burning or stinging sensation on your feet, especially in the areas affected by athlete’s foot, it could be a sign of the infection worsening. This discomfort is often exacerbated by friction from wearing shoes and can be quite bothersome.
Development of Blisters
In some cases, athlete’s foot can lead to the formation of blisters on the affected skin. These blisters may be filled with fluid and can cause additional discomfort and pain, particularly when they rupture or rub against shoes or socks.
Dry, Scaly Skin on the Bottom of the Foot Extending Up the Side
Athlete’s foot can also manifest as dry, scaly skin on the bottom of the foot, which may extend up the sides. This occurs when the infection spreads or if the fungus affects multiple areas of the foot, leading to widespread skin irritation and flakiness.
Conclusion:
Athlete’s foot, caused by fungi thriving in warm, moist environments, presents with symptoms like peeling skin, persistent itchiness, inflammation, burning sensation, blisters, and dryness. Effective management involves keeping the feet clean and dry, wearing breathable footwear, and using antifungal treatments as needed to alleviate discomfort and promote healing.
more about Athlete’s Foot
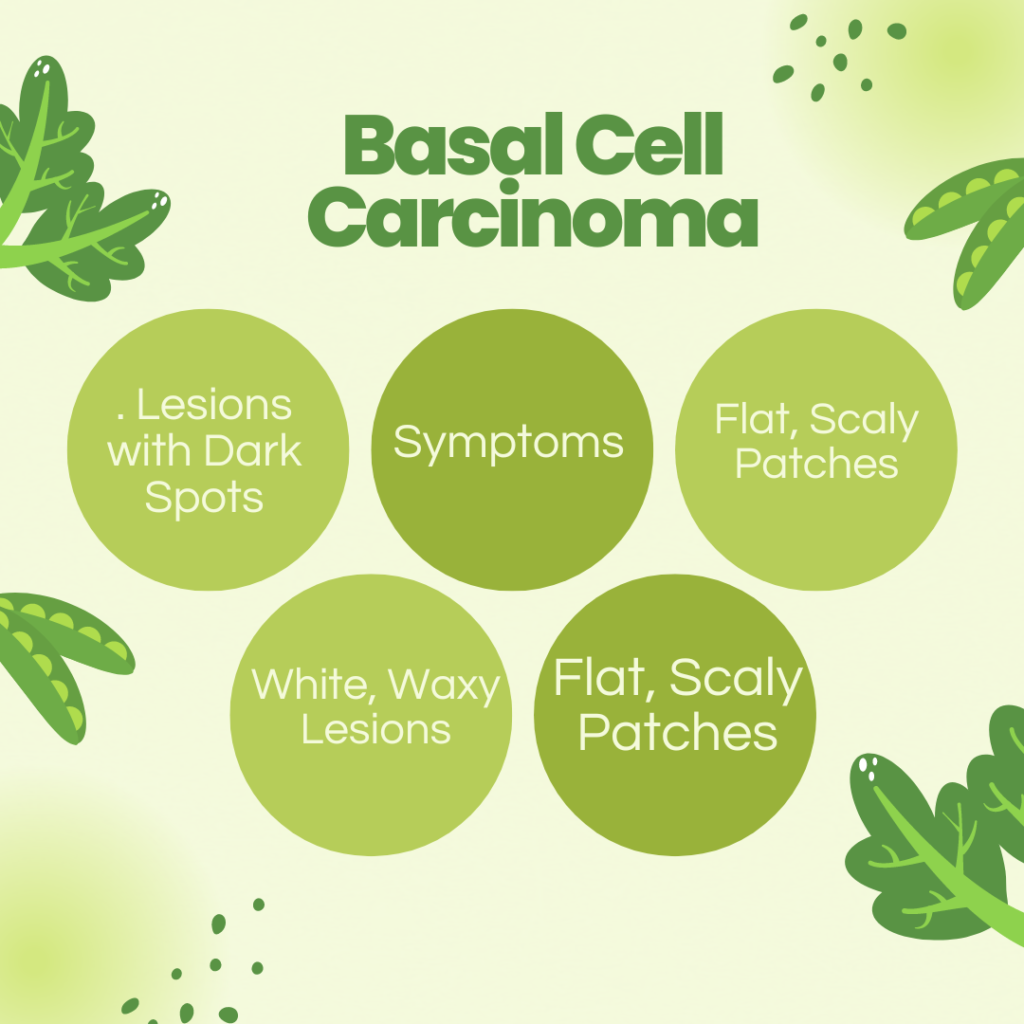
Basal Cell Carcinoma:
When something goes wrong with these basal cells, they can start growing out of control, forming a bump or lesion on the skin. This bump might look slightly transparent, but it can also take on other shapes and forms. It often shows up on areas of the skin that get a lot of sun exposure, like the head and neck.
Why Basal Cell Carcinoma Happens:
Basal cell carcinoma likes to hang out in places where the sun shines the most, like your head and neck. That’s because long-term exposure to sunlight, specifically the UV radiation it gives off, is often the cause of this type of cancer.(Eczema, Acne, Shingles, etz are the Common skin infections.)
Symptoms:
Shiny, Translucent Bumps
One common sign of skin cancer is a shiny bump on the skin that’s translucent, meaning you can see through it a bit. On lighter skin, it might look pearly white or pink, while on darker skin, it could appear brown or glossy black. Sometimes, tiny blood vessels are visible. If the bump bleeds and scabs over, it’s important to take notice.
Lesions with Dark Spots
Another sign to watch out for is a lesion that’s brown, black, or blue, or has dark spots. These lesions might have a slightly raised, translucent border. They can vary in color and appearance, but any unusual spots on the skin should be checked out by a doctor.
Flat, Scaly Patches
Skin cancer can also present as flat, scaly patches with a raised edge. These patches may start small but can grow larger over time if left untreated. It’s essential to pay attention to any changes in the skin’s texture or appearance.
White, Waxy Lesions
Lastly, some skin cancers may appear as white, waxy, scar-like lesions without a clearly defined border. These lesions can be easy to overlook, especially if they blend in with the surrounding skin. However, any unusual marks on the skin should be evaluated by a healthcare professional.
Effective Solutions for Relief:
Keep the Affected Area Clean and Dry
First things first, it’s essential to keep the area affected by basal cell carcinoma clean and dry.Tenderly wash the zone with mellow cleanser and water, at that point pat it dry with a clean towel. Keeping the zone clean can offer assistance avoid contamination and advance recuperating.
Use Moisturizers
Moisturizers can help soothe dry, irritated skin caused by basal cell carcinoma. Hunt for moisturizers that are fragrance-free and tender on the skin.Applying moisturizer regularly can help keep the skin hydrated and reduce itching and discomfort.
Avoid Scratching or Picking at the Lesions
It can be tempting to scratch or pick at the lesions caused by basal cell carcinoma, but this can worsen the condition and increase the risk of infection. Try to resist the urge to scratch or pick at the affected area. If itching is a problem, applying a cold compress or using over-the-counter anti-itch creams can help provide relief.
4. Protect the Skin from Sun Exposure
Since sun exposure is a major risk factor for basal cell carcinoma, it’s essential to protect the skin from the sun’s harmful rays. Wear protective clothing, such as long-sleeved shirts and wide-brimmed hats, when outdoors, and use sunscreen with a high SPF. Limiting sun exposure, especially during peak hours, can help prevent further damage to the skin.
Conclusion:
Basal Cell Carcinoma (BCC) is a common skin cancer triggered by abnormal growth of basal cells, often appearing as translucent bumps or dark lesions due to sun exposure. To manage BCC, keep the affected area clean, use moisturizers, avoid scratching, and protect from the sun. Early detection and preventive measures are crucial for minimizing its impact on health.
more about Basal Cell Carcinoma


1 thought on “Common skin infections: Causes, Symptoms, and Treatments.”